Optimizing Treatments for Favorable Outomes
“Testicular Cancer is the Model of a Curable Neoplasm” Dr. Einhorn, 1981
Early detection via awareness and access to care by being insured are futile if unfavorable outcomes occur because of less than optimal treatments.
Unfavorable outcomes can occur for many reasons: late diagnosis, misinterpretation of pathology, imaging studies or tumor markers, mis-assignment of risk category, misuse or over use of imaging modalities, inconsistent delivery of chemotherapy, suboptimal Retroperitoneal Lymph Node Dissections and even mortalities from unnecessary treatments.
We are certainly not saying that individual doctors are not capable of treating testicular cancer patients but treatment or oversight by more experienced physicians can help assure better outcomes. High volume centers see larger numbers of testicular cancer patients and have surgeons, pathologists and medical oncologists that have extensively focused their careers on testicular cancer. Their experience breeds familiarity with various guidelines, the ability to customize treatments for each patient and the case experience to confidently make the tough clinical decisions.
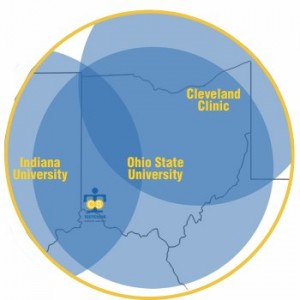
Every Guy in Ohio is Within a Few Hours Drive of High Volume, World-Renowned Testicular Cancer Experts and Treatment Teams.
The Testicular Cancer Resource Center maintains a list of experts in the field of testicular cancer, which includes the programs at Indiana University and Cleveland Clinic. Likewise, The James at Ohio State University is a National Cancer Institute designated Comprehensive Cancer Center.
We highly recommend to treating physicians that if they have a patient diagnosed at a late stage or that has not responded to initial treatment that they seek advice from one of these experts.
A recent look at stage III testicular cancer patients from 1998 – 2011 showed that patients treated at higher volume centers had better mortality outcomes. Center volumes were classified by quartiles of 1-5, 6-10, 11-60 or > 60 testicular cancer patients diagnosed per hospital per year. Better survival outcomes were observed in relationship to hospital volume and were most evident in centers that saw 5 or less vs. > 60 testicular cancer patients per year. The media number of testicular cancer patients seen per hospital per year was 8 with a dramatic range of 1-115 patients seen per year.
We highly recommend that Retroperitoneal Lymph Node Dissection (RPLND) be done by high volume expert surgeons.
Data from 2001-2008 indicate that over half of the RPLNDs are done in hospitals that perform 2 or fewer RPLNDs per year. A recent study indicated that for those applying for certification with the American Board of Urology from 2003 to 2013 only 3.4% of urologists documented doing a RPLND in their case logs. Of those that did log an RPLND, 75% logged the equivalent of 2 RPLNDs per year. Over 50% of all RPLNDs were done by surgeons that logged the equivalent of 4 or less RPLNDs per year. Three urologists logged 23% of all the RPLND cases showing a dramatic difference in individual surgeon volumes ranging from 2 to 118 RPLNDs per year.
Recently diagnosed?
Have you or someone you know been recently diagnosed with testicular cancer? If so, contact us or call the Testicular Cancer Society at 513-696-9827 to make sure all of the available resources for testicular cancer are at your disposal.
Second Opinion or Referring a Patient?
If you are a patient wanting a second opinion or a physician looking to refer a patient to a high volume center then contact us or call the Testicular Cancer Society at 513-696-9827 and we are more than happy to assist you.
Get Involved & Join #TalkAboutTC
Let’s end deaths from testicular cancer
Not ready to join?
Why not stay updated and decide later
We promise not to blow up your inbox.

